Bunion Treatment

Bunions are a common foot deformity where the joint at the base of the big toe becomes enlarged and misaligned, causing the toe to angle inward. This can lead to pain, swelling, and difficulty in finding comfortable shoes. The condition often develops due to genetic factors, wearing ill-fitting footwear, or arthritis. If you have bunions, it is essential to take proactive steps to manage the discomfort and prevent further progression. Start by wearing shoes with a wide-toe box, low heels, and good arch support. Regularly performing foot exercises to strengthen the muscles around the joint can also provide relief. If these conservative measures do not help, or if the bunion becomes severely painful, it is suggested that you consult a podiatrist. In some cases, surgery may be recommended to correct the deformity and restore foot function.
If you are suffering from bunions, contact Pasquale Cancelliere, DPM of Candria Foot and Ankle Specialists. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
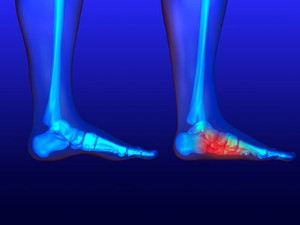
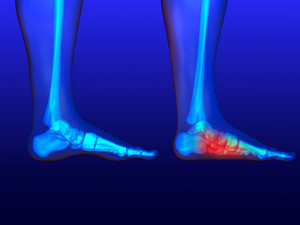
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our offices located in Londonderry, NH and Salem, NH . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is an enlargement of the base joint of the toe that connects to the foot, often formed from a bony growth or a patch of swollen tissues. It is caused by the inward shifting of the bones in the big toe, toward the other toes of the foot. This shift can cause a serious amount of pain and discomfort. The area around the big toe can become inflamed, red, and painful.
Bunions are most commonly formed in people who are already genetically predisposed to them or other kinds of bone displacements. Existing bunions can be worsened by wearing improperly fitting shoes. Trying to cram your feet into high heels or running or walking in a way that causes too much stress on the feet can exacerbate bunion development. High heels not only push the big toe inward, but shift one's body weight and center of gravity towards the edge of the feet and toes, expediting bone displacement.
A podiatrist knowledgeable in foot structure and biomechanics will be able to quickly diagnose bunions. Bunions must be distinguished from gout or arthritic conditions, so blood tests may be necessary. The podiatrist may order a radiological exam to provide an image of the bone structure. If the x-ray demonstrates an enlargement of the joint near the base of the toe and a shifting toward the smaller toes, this is indicative of a bunion.
Wearing wider shoes can reduce pressure on the bunion and minimize pain, and high heeled shoes should be eliminated for a period of time. This may be enough to eliminate the pain associated with bunions; however, if pain persists, anti-inflammatory drugs may be prescribed. Severe pain may require an injection of steroids near the bunion. Orthotics for shoes may be prescribed which, by altering the pressure on the foot, can be helpful in reducing pain. These do not correct the problem; but by eliminating the pain, they can provide relief.
For cases that do not respond to these methods of treatment, surgery can be done to reposition the toe. A surgeon may do this by taking out a section of bone or by rearranging the ligaments and tendons in the toe to help keep it properly aligned. It may be necessary even after surgery to wear more comfortable shoes that avoid placing pressure on the toe, as the big toe may move back to its former orientation toward the smaller toes.
Causes and Prevention Tips for Foot Stress Fractures

A foot stress fracture is a small crack in a bone, typically resulting from repetitive force or overuse. This injury commonly occurs in athletes or individuals who suddenly increase their physical activity without adequate preparation. Factors contributing to stress fractures include wearing improper footwear, inadequate training techniques, and sudden changes in exercise intensity. Symptoms often involve localized pain that worsens with activity and improves with rest. To prevent foot stress fractures, it is essential to gradually increase activity levels, choose supportive footwear, and incorporate proper warm-up and stretching routines. Strengthening exercises for the foot and lower leg can also help build resilience. If you have sustained a foot stress fracture, it is suggested that you schedule an appointment with a podiatrist who can treat this condition.
Stress fractures occur when there is a tiny crack within a bone. To learn more, contact Pasquale Cancelliere, DPM from Candria Foot and Ankle Specialists. Our doctor can provide the care you need to keep you pain free and on your feet.
How Are They Caused?
Stress fractures are the result of repetitive force being placed on the bone. Since the lower leg and feet often carry most of the body’s weight, stress fractures are likely to occur in these areas. If you rush into a new exercise, you are more likely to develop a stress fracture since you are starting too much, too soon. Pain resulting from stress fractures may go unnoticed at first, however it may start to worsen over time.
Risk Factors
- Gender – They are more commonly found in women compared to men.
- Foot Problems – People with unusual arches in their feet are more likely to develop stress fractures.
- Certain Sports – Dancers, gymnasts, tennis players, runners, and basketball players are more likely to develop stress fractures.
- Lack of Nutrients – A lack of vitamin D and calcium may weaken the bones and make you more prone to stress fractures
- Weak Bones – Osteoporosis can weaken the bones therefore resulting in stress fractures
Stress fractures do not always heal properly, so it is important that you seek help from a podiatrist if you suspect you may have one. Ignoring your stress fracture may cause it to worsen, and you may develop chronic pain as well as additional fractures.
If you have any questions, please feel free to contact our offices located in Londonderry, NH and Salem, NH . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Stress Fractures of the Foot and Ankle
Our bones are important aspects of our body and they are constantly changing. The heavier the workload for a bone, the more likely it is that calcium will be placed in it. When a bone isn’t used often, there won’t be much calcium within it. When stress from repetitive loads prevent the bone from being able to repair itself, cracks will start to form. Stress fractures are defined as cracks in a bone that result from repetitive force, such as overuse.
The most common cause of stress fractures is a sudden increase in intensity and duration of physical activity. For example, if you begin to run long distances without working your way into doing so, you will be more likely to develop a stress fracture.
Common symptoms of stress fractures are pain and swelling near the weight bearing area on the injured bone. When initial x-rays are performed, it is possible that the fracture will not show up. However, once the stress on the area continues, the damage will increase, and the fracture will be severe enough to show up on an x-ray. Certain parts of the foot are more likely to develop stress fractures than others. Areas that typically have these fractures are: the metatarsals, the navicular bone, the calcaneus, tibia, and fibula.
Since women are at an increased risk of developing osteoporosis, they are twice as likely as men to sustain a stress fracture. Additionally, old age causes a decrease in bone mineral density which is why elderly people are also likely to develop these fractures.
It is important for you to be professionally diagnosed by a podiatrist if you suspect you have a stress fracture, because there are other injuries that can easily be mistaken for a fracture. Sprains, strains, shin splints, plantar fasciitis, and Morton’s neuroma can all easily be mistaken for stress fractures in the foot. Your podiatrist will likely ask you a series of questions to determine what type of pain you are experiencing. These questions will help your doctor identify whether you have a stress fracture.
The best method of treatment for a stress fracture is rest. Additionally, a walking boot, cast, or crutches, will help rest the area that is injured. The typical healing time for stress fractures is 4-12 weeks, however this depends on which bone is involved.
Keep Your Feet Healthy So You Can Stay Active
Facts About Flat Feet
Flat feet, or pes planus, come in two main types, which are flexible and rigid. Flexible flat feet show arches that flatten when standing but are visible when sitting, while rigid flat feet have no arch even when sitting. Symptoms often include foot pain, swelling, and difficulty walking or standing for long periods. Risk factors include genetic predisposition, obesity, and certain medical conditions like arthritis. To alleviate discomfort, specific stretches can be helpful. Stretching the Achilles tendon and calf muscles can relieve tension and improve foot flexibility. Foot exercises, such as toe curls and arch lifts, strengthen the muscles supporting the arch. If you have flat feet, it is strongly suggested that you are under the care of a podiatrist who can offer effective relief solutions.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Pasquale Cancelliere, DPM from Candria Foot and Ankle Specialists. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our offices located in Londonderry, NH and Salem, NH . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flatfoot
Flatfoot is a foot disorder that is not as straightforward as many people believe. Various types of flatfoot exist, each with their own varying deformities and symptoms. The partial or total collapse of the arch, however, is a characteristic common to all types of flatfoot. Other signs of flatfoot include:
- “Toe drift,” or the pointing outward of the toes and the front part of the foot
- The tilting outward of the heel and the tilting inward of the ankle
- The lifting of the heel off the ground earlier when walking due to a tight Achilles tendon
- Hammertoes
- Bunions
One of the most common types of flatfoot is flexible flatfoot. This variation usually starts in childhood and progresses as one ages into adulthood. Flexible flatfoot presents as a foot that is flat when standing, or weight-bearing. When not standing, the arch returns. Symptoms of flexible flatfoot include:
- Pain located in the heel, arch, ankle, or along the outside of the foot
- Overpronation, or an ankle that rolls in
- Shin splint, or pain along the shin bone
- General foot aches or fatigue
- Pain located in the lower back, hip, or knee
Your podiatrist will most likely diagnose flatfoot by examining your feet when you stand and sit. X-rays may be taken to define the severity and help determine the treatment option best for your condition. Nonsurgical treatments can include activity modification, weight loss, orthotics, immobilization, medications, physical therapy, shoe modifications, and ankle foot orthoses (AFO) devices. If nonsurgical methods prove ineffective, surgery may be considered. Multiple surgical procedures can correct flatfoot; and depending on your specific condition, one may be selected alone or combined with other techniques to ensure optimal results.
Stages of Toenail Fungus

Toenail fungus progresses through distinct stages, each requiring timely intervention. In the earliest stage, the nail may appear slightly discolored, usually yellow or white, with minimal discomfort. Without treatment, the condition advances to the moderate stage, where the nail becomes thicker and more discolored, and may develop a crumbly texture. This stage often involves some pain or discomfort. If untreated, toenail fungus can reach an advanced stage, causing severe thickening, distortion, and detachment of the nail from the nail bed. This stage can lead to significant pain and difficulty walking. In the chronic stage, the infection is longstanding and difficult to treat, potentially leading to permanent damage. If you notice the beginning stages of toenail fungus, it is suggested that you consult a podiatrist who can offer you effective treatment options which may prevent advancing to later stages.
For more information about treatment, contact Pasquale Cancelliere, DPM of Candria Foot and Ankle Specialists. Our doctor can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please feel free to contact our offices located in Londonderry, NH and Salem, NH . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Toenail Fungus
Toenail fungus is a frustrating problem that affects many people. It can be persistent and hard to get rid of. As many different types of fungi are present throughout the environment, it is very easy to contract toenail fungus.
The feet are especially susceptible to toenail fungus because shoes and socks create the ideal dark and moist environment that fungal infections thrive in. While fungal infections of the nail plate are quite common, if left untreated they can spread beyond the toenail and into the skin and other parts of the body.
Signs of toenail fungus include a thickened nail that has become yellow or brown in color, a foul smell, and debris beneath the nail. The toe may become painful due to the pressure of a thicker nail or the buildup of debris.
Treatment for toenail fungus is most effective during the early stages of an infection. If there is an accumulation of debris beneath the nail plate, an ingrown nail or a more serious infection can occur. While each treatment varies between patients, your podiatrist may prescribe you oral medications, topical liquids and creams, or laser therapy. To determine the best treatment process for you, be sure to visit your podiatrist at the first signs of toenail fungus.
Osteoarthritis of the Ankle
 Ankle osteoarthritis is a relatively uncommon condition often arising years after an ankle injury that damages the cartilage. Unlike other forms of arthritis, it tends to affect younger individuals, especially those with a history of trauma to the joint. Excess weight can worsen the condition by increasing stress on the ankle and accelerating cartilage deterioration. Symptoms of ankle osteoarthritis include pain, stiffness, and swelling in the joint, which can increase with activity and improve with rest. Patients may also experience a reduced range of motion and a feeling of instability in the ankle. Diagnosis typically involves a physical examination, patient history, and imaging tests, such as X-rays or MRI scans, to assess cartilage damage and joint space narrowing. Treatment focuses on managing symptoms and improving joint function. Conservative approaches include weight management, targeted stretching exercises, anti-inflammatory medications, and orthotics. In severe cases, surgical options like ankle arthroscopy, fusion, or joint replacement may be considered to alleviate pain and restore mobility. If you have persistent ankle pain, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment.
Ankle osteoarthritis is a relatively uncommon condition often arising years after an ankle injury that damages the cartilage. Unlike other forms of arthritis, it tends to affect younger individuals, especially those with a history of trauma to the joint. Excess weight can worsen the condition by increasing stress on the ankle and accelerating cartilage deterioration. Symptoms of ankle osteoarthritis include pain, stiffness, and swelling in the joint, which can increase with activity and improve with rest. Patients may also experience a reduced range of motion and a feeling of instability in the ankle. Diagnosis typically involves a physical examination, patient history, and imaging tests, such as X-rays or MRI scans, to assess cartilage damage and joint space narrowing. Treatment focuses on managing symptoms and improving joint function. Conservative approaches include weight management, targeted stretching exercises, anti-inflammatory medications, and orthotics. In severe cases, surgical options like ankle arthroscopy, fusion, or joint replacement may be considered to alleviate pain and restore mobility. If you have persistent ankle pain, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact Pasquale Cancelliere, DPM from Candria Foot and Ankle Specialists. Our doctor can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a term that is commonly used to describe joint pain. The condition itself can occur to anyone of any age, race, or gender, and there are over 100 types of it. Nevertheless, arthritis is more commonly found in women compared to men, and it is also more prevalent in those who are overweight. The causes of arthritis vary depending on which type of arthritis you have. Osteoarthritis for example, is often caused by injury, while rheumatoid arthritis is caused by a misdirected immune system.
Symptoms
- Swelling
- Pain
- Stiffness
- Decreased Range of Motion
Arthritic symptoms range in severity, and they may come and go. Some symptoms stay the same for several years but could potentially get worse with time. Severe cases of arthritis can prevent its sufferers from performing daily activities and make walking difficult.
Risk Factors
- Occupation – Occupations requiring repetitive knee movements have been linked to osteoarthritis
- Obesity – Excess weight can contribute to osteoarthritis development
- Infection – Microbial agents can infect the joints and trigger arthritis
- Joint Injuries – Damage to joints may lead to osteoarthritis
- Age – Risk increases with age
- Gender –Most types are more common in women
- Genetics – Arthritis can be hereditary
If you suspect your arthritis is affecting your feet, it is crucial that you see a podiatrist immediately. Your doctor will be able to address your specific case and help you decide which treatment method is best for you.
If you have any questions, please feel free to contact our offices located in Londonderry, NH and Salem, NH . We offer the newest diagnostic and treatment technologies for all your foot care needs.